Module 1: EMR Technology Overview
Learning Objectives
Upon completion of this module, you will be able to:
- Recognize that EMR is much more than an eChart, and that it is a powerful technology that can be used to improve patient care and prescribing;
- Describe current and emerging benefits of EMR and its capabilities to support chronic disease management and preventive care.
Introduction to EMR Capabilities
EMR is a technology used by healthcare providers to capture and record patient chart information. It encompasses practice management capabilities such as schedules of appointments, patient demographic information, and an interface to provincial Ministries of Health for the electronic submission of claims. It is also a workflow instrument that supports providers and staff to manage and coordinate patient-level and practice-level tasks; for example, the ordering of a laboratory investigation or a patient recall.
Patient records include visit notes, medical and pharmaceutical history, allergies, vaccinations, and diagnostic information such as laboratory results and findings from imaging studies. In addition, records hold care plans organized according to the individual patient or to the state of disease for all patients. Some EMRs includes patient or population goals based upon system or provider established criteria such as age, gender, and medical profile.
How EMR Can Improve Clinical Care
EMR can be much more than an electronic version of a paper chart. Particularly as readily searchable software that captures structured data (i.e., organized and coded data vs. free [unstructured] text), EMR serves as an information system that can be used by providers and staff to preventively, proactively, and reactively improve clinical outcomes. Through the use of search-and-recall capabilities, providers can identify patient populations of interest and initiate recommended care such as screening or vaccination. Providers can integrate evidence into practice through the use of such tools as documented care plans, evidence-based encounter templates that mine the EMR for contextual data (e.g., latest HgA1c for a diabetic visit), therapeutic goal monitoring, and strategically placed clinical decision supports and alerts. These tools allow providers to opportunistically deliver appropriate and timely care when seeing patients for any condition.
EMR technology can also improve communication and coordination between providers and the broader healthcare system. More effective inter-professional communication is achieved when tasks (e.g., a consultation request from a GP to a specialist, called an e-Referral), as well as patient data (e.g., previous results from investigations or visit notes, called data sharing) can be electronically transmitted. More broadly, entire care teams can be included in care plans stored and executed via EMR for optimal and highly effective collaboration. Finally, the technology allows providers to obtain relevant patient information, (e.g., results from investigations or patient encounter reports from other healthcare system sectors) directly into their EMR, often as discrete data. They then have all the required information to make informed medical decisions at the point of care.
Benefits of EMR Use in Canada
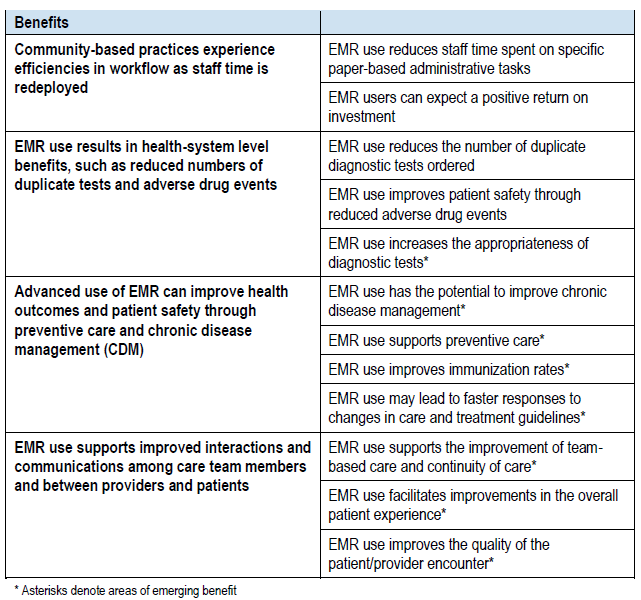
Canada Health Infoway2 as presented in Table 1, has articulated a number of key current and emerging benefits of EMR use in Canada.
Table 1: Current and Emerging Benefits of EMR Use in Canada
EMR Capabilities to Support CDM and Preventive Care
With respect to EMR capabilities to support chronic disease management (CDM) and prevention, Hillestad et al., as cited by Canada Health Infoway2, has highlighted that EMRs are useful in:
- Identifying people with active or potential chronic disease;
- Targeting services to patients based on their level of risk. Sicker patients can benefit from more tailored, more intensive interventions;
- Monitoring conditions. Condition-specific encounter templates implemented in an EMR system can ensure consistent recording of disease-specific clinical results, leading to better clinical decisions and outcomes;
- Improving screening and testing by tracking the frequency of preventive services and reminding physicians to offer recommended tests;
- Modifying patient behaviour. Electronic messaging offers a low-cost, efficient means of distributing reminders to patients and responding to patient inquiries. Also, web-based patient education can increase the patient’s knowledge of a disease and compliance with protocols;
- Adjusting therapy (e.g., based on the use of easily accessible and regularly updated guidelines);
- Improving case management for higher-risk patients (e.g., enhancing communication between multiple specialists and patients); and
- Connecting to national disease registries to allow practices to compare their performance with that of others.
Canada Health Infoway2 cites a number of studies and concludes that the literature has shown preventive care to be an area where EMR can have a substantial positive impact:
In a systematic review of controlled health information system studies, Lau et al. found that 72% of studies had positive results using preventive care reminders, mostly through guideline adherence such as immunization and health screening. In another systematic review focused on the impact of EMRs specifically, Lau et al. found that preventive care had the most positive findings (about 67% of studies showed a positive effect of EMRs).
Canada Health Infoway in the same report concluded that findings related to EMR use supporting chronic disease management (CDM) have been mixed. It was suggested that the apparent conflicting findings “may be a result of the sophistication of each EMR and whether all available functionalities are being used on a regular basis and when the functionalities that support CDM are in use (e.g., population-based reminders and decision support), there are significant benefits to be realized.” Based on the literature, they further found overall immunization rates do increase with the use of EMR, and that “EMR use may lead to faster responses to changes in care and treatment guidelines (for example, for changes to medication guidelines, physicians using EMR can more proficiently generate reports of patients currently taking specific medications without having to sort through hundreds of paper charts).”
The potential for EMR to improve preventive and chronic disease management care is very important for the life sciences industry. Effective implementation of the various EMR decision-support tools permit healthcare professionals to better provide evidence-based care. This often will have a direct positive correlation on the prescribing of appropriate treatments, especially newer therapies. In many therapeutic categories, there is often not a knowledge gap (what to do per the evidence or clinical guidelines), but rather an action gap, as physicians don’t have the tools to support putting evidence into practice. When used with a level of maturity, EMR is an important technology with which to close this gap.
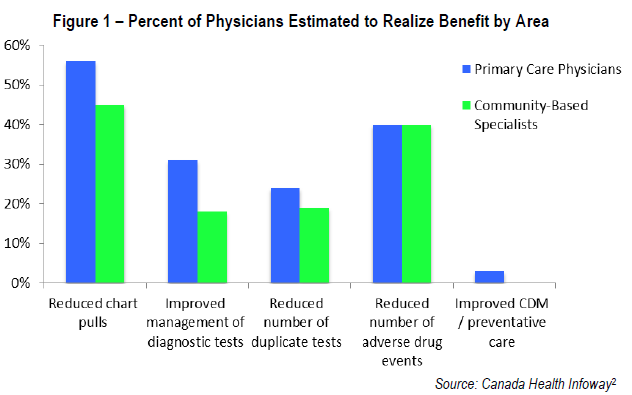
As discussed later in this course, and as Figure 1 notes, there is much work to be done to support physicians and other healthcare professionals and their staff in realizing a proficient and mature level of EMR utilization.
Key Summary Points
- EMR is a powerful technology that can be much more than an electronic version of a paper chart.
- EMR serves as an information system that providers and staff can use to preventively, proactively, and reactively improve clinical outcomes.
- A number of studies have concluded that preventive care is an area where EMR can have a substantial positive impact.
- Findings related to EMR use supporting chronic disease management (CDM) have been mixed; however, when the functionalities that support CDM are in use (e.g., population-based reminders and decision support), there are significant benefits realized.
- There is much work to be done to support physicians and other healthcare professionals and their staff in realizing a proficient and mature level of EMR utilization.
- The potential for EMR to improve care is very important for industry. Effective implementation of the various EMR tools and decision-support capabilities permits healthcare professionals to better provide evidence-based care. This often will have a direct positive correlation on the prescribing of appropriate therapies, especially newer innovations.
Module Progress Check
1. When used with a level of maturity, EMR is more than an electronic version of a paper chart.
a) True
b) False
2. Healthcare professionals and staff have a high level of proficiency and maturity in EMR utilization.
a) True
b) False
3. EMR is a tool to:
a) Record patient chart information
b) Manage workflow between different providers and staff within a clinic
c) Receive and document results from investigations such as laboratory tests
d) All of the above
4. EMR data is readily searchable, permitting the software to be used as a clinical information system when data is entered as structured data.
a) True
b) False
Module Answers
-
- True
- False
- d
- True
